The Science of Lactation and Fertility: When will I get my period back if I’m breastfeeding?
The Science of Lactation and Fertility: When will I get my period back if I’m breastfeeding, chestfeeding or lactating?
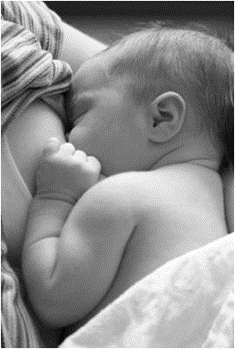
For many breastfeeding moms, lactational amenorrhea is a pretty darn nice perk. With my firstborn, I was one of the lucky ones—I went an entire year after my baby was born without getting a period thanks to breastfeeding. It would be an understatement to say I was delighted the entire time. In fact, I seriously considered adding in some extra pumping after year 1 just to keep that lovely little side effect.
Second baby, I was excitedly anticipating another 2 years period free—yippee!!! So imagine my surprise when at 7 and a half months postpartum, my period returned. I was supposed to get a full year—just like last time!
Now, as I understood lactational amenorrhea theory at the time, the loss of fertility during lactation was due to the frequency of suckling or nursing intensity. According to this theory, the more often you feed the baby, the less likely you are to ovulate.1-2 While this makes sense in many cases, in my own experience it didn’t add up. As I was often home with him, I nursed my second baby much more often than I nursed my first (I was working full time and pumping), but my periods returned more than 5 months sooner.
While researching lactational amenorrhea for a review article with colleagues, I came across a study with an alternate theory called the metabolic load hypothesis. Valeggia and Ellison found that in a group of Toba women in Argentina who had high nursing intensity and high nutritional status they could predict the return of menses by looking at a mother’s energy balance rather than just nursing intensity.3 They were looking at this equation:
Total energy taken in (eating) – Total energy used up (breastfeeding, exercise)
When this equation came out to a positive number (more energy in than energy out), the authors could actually detect a rise in C peptide levels (a marker for insulin) in a women’s urine, and soon after, that woman “got her period back.”
When I think about my situation using this theory, it makes a little more sense. With my first, although I went back to work full time at 3 months, my job as a graduate student in a cell biology lab was pretty physically active. Despite sitting down a bit here and there, I was frequently standing up, lifting, walking across the lab to get something and moving my body to conduct my experiments. In addition, I was pumping every 3 hours or so while I was away from my baby. My energy output was more than my energy input up until the time friends convinced me to stop pumping at work a little after my son was a year old. Within a month my period had returned.
With my second baby, I worked part time and had a more flexible schedule, allowing me to work at home often and be close by to nurse my son on demand much of the time rather than deal with pumping. While this situation provided for greater nursing intensity, my energy expenditure was much lower than it had been as a graduate student. In contrast to the constant movement I experienced working in the lab, as a professor I spent much of my work time sitting and writing on the computer, and sometimes snacking while I was doing that. Not a good recipe for expending energy!
Given the differences in my activity level while nursing my 2 children, the very different timing I experienced in return of menses starts to make sense.
Although most of us (myself included) generally think about this in terms of the physical signals of menses–getting our periods back— what’s really happening is ovulation. You may have heard that high performance athletes often stop menstruating when they’re training really intensely? Scientists believe that intense energy expenditure or lack of food act as a signal to the body that it’s not a good time to reproduce, causing the body to shut down ovulation. Making and raising babies takes a tremendous amount of resources—not something mom has if she’s starving or expending huge amounts of energy, such as in training for the Olympics.
According to the metabolic load hypothesis, lactational amenorrhea may work much the same way. Milk making in humans requires an average of 500 extra calories a day, even more than pregnancy. If mom is exclusively breastfeeding and active, her energy output through activity and lactation is likely to be greater than or equal to her energy input. If baby starts nursing less, mom becomes less active, or starts consuming more calories than she needs, her body gets the signal that there are ample resources to have more babies, and mom starts ovulating (and menstruating) again.
The average duration of lactational amenorrhea in exclusively breastfeeding (no formula, foods, or anything else) mothers in the US is about 6 months.4 This coincides fairly well with the start of the introduction of solid foods, which may begin to reduce nursing intensity. Before then, the lactational amenorrhea method can even be used as a form of birth control, believed to be about 98% effective provided you follow these rules:5-6
Lactational Amenorrhea Method
1. Baby must be less than 6 months old.
2. Mom must not have had a return of menses (defined as 2 contiguous days of bleeding, 2 contiguous days of spotting and 1 day of bleeding, or 3 contiguous days of spotting)
3. Mom is exclusively breastfeeding her baby with no more than 4 hours between daytime feeds and no more than 6 hours between night time feeds and no more than 10% of calories coming from supplementation with infant formula or complementary food5-6
As for me, I’m glad there’s data to explain my experience!
When did you get your period back while breastfeeding? Did it differ between children?
1. C.C.K Tay AG, A. McNeilly. Twenty-four hour patterns of prolactin secretion during lactation and the relationship to suckling and the resumption of fertility in breast-feeding women. Human Reproduction 1996;11(5):950-955.
2. McNeilly AS, Tay CCK, Glasier A. Physiological Mechanisms Underlying Lactational Amenorrhea. Annals of the New York Academy of Sciences 1994;709(1):145-155.
3. Valeggia C, Ellison PT. Interactions between metabolic and reproductive functions in the resumption of postpartum fecundity. Am J Hum Biol 2009;21(4):559-66.
4. Heinig MJ N-RL, Peerson JM, Dewey KG. Factors related to duration of postpartum amenorrhoea among USA women with prolonged lactation. J Biosoc Sci. 1994;26(4):517-27.
5. Hight-Laukaran V, Labbok MH, Peterson AE, Fletcher V, von Hertzen H, Van Look PFA. Multicenter study of the Lactational Amenorrhea Method (LAM): II. Acceptability, utility, and policy implications. Contraception 1997;55(6):337-346.
6. Peterson AE, Peŕez-Escamilla R, Labboka MH, Hight V, von Hertzen H, Van Look P. Multicenter study of the lactational amenorrhea method (LAM) III: effectiveness, duration, and satisfaction with reduced client–provider contact. Contraception 2000;62(5):221-230.